Juvenile Diabetes and Puberty: Hormonal Challenges
Juvenile diabetes, also known as type 1 diabetes, presents unique difficulties when combined with the transformative phase of puberty. Juvenile Diabetes and Puberty: Hormonal Challenges is a topic that affects thousands of families worldwide, as the surge in hormones during adolescence can significantly disrupt blood sugar control and insulin needs. This article explores Juvenile Diabetes and Puberty: Hormonal Challenges in depth, examining the physiological mechanisms, management strategies, and real-life experiences to help parents, teens, and caregivers navigate this critical period.
Understanding Juvenile Diabetes and Puberty: Hormonal Challenges begins with recognizing that type 1 diabetes is an autoimmune condition where the pancreas produces little to no insulin, requiring lifelong management through injections or pumps. When puberty arrives, typically between ages 8–13 in girls and 9–14 in boys, the body undergoes rapid changes driven by hormones, amplifying the difficulties of Juvenile Diabetes and Puberty: Hormonal Challenges. These hormonal shifts often lead to increased insulin resistance, unpredictable blood glucose levels, and higher risks of complications if not addressed promptly.
What Is Juvenile Diabetes?
Juvenile diabetes, or type 1 diabetes, usually emerges in childhood or adolescence. The immune system attacks insulin-producing beta cells in the pancreas, leading to insulin deficiency. Symptoms include excessive thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision. Diagnosis often occurs through blood tests showing high glucose and autoantibodies.
In the context of Juvenile Diabetes and Puberty: Hormonal Challenges, early diagnosis is crucial because uncontrolled diabetes can delay puberty or affect growth. With modern insulin therapies, most individuals achieve normal development, but Juvenile Diabetes and Puberty: Hormonal Challenges remain prominent during the teenage years.
Puberty: A Time of Profound Hormonal Changes
Puberty marks the transition from childhood to adulthood, involving surges in growth hormone (GH), sex hormones (estrogen in girls, testosterone in boys), and others like cortisol and leptin. These changes drive growth spurts, sexual maturation, and brain remodeling. In healthy teens, insulin sensitivity fluctuates, but the body compensates.
For those with juvenile diabetes, Juvenile Diabetes and Puberty: Hormonal Challenges intensify because the lack of natural insulin production makes compensation difficult. Insulin requirements can rise by 30–50%, and blood sugar swings become more pronounced.
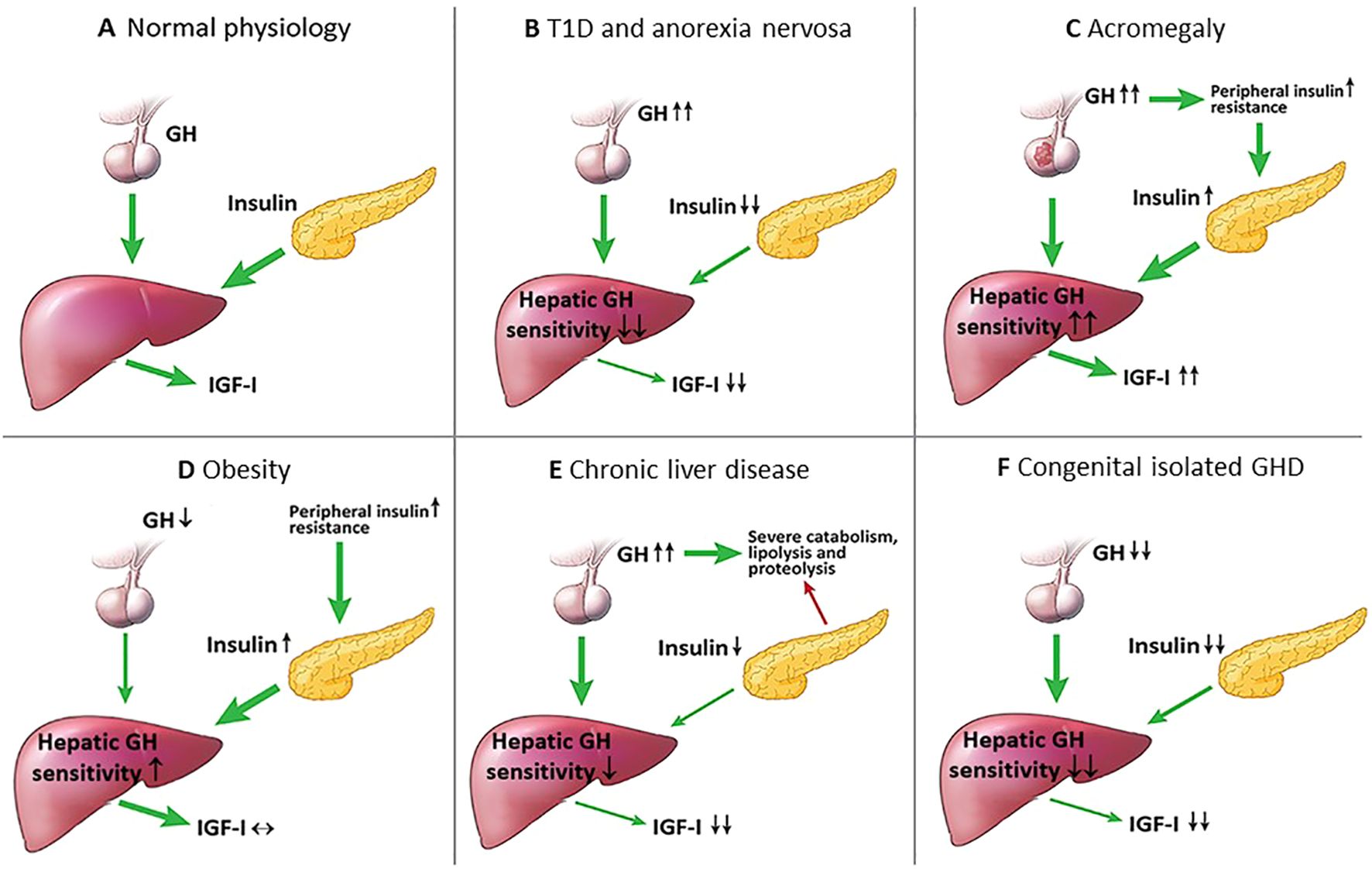
This illustration depicts the growth hormone/insulin-like growth factor-1 (IGF-1) axis in type 1 diabetes, highlighting how reduced portal insulin leads to lower IGF-1 and increased GH secretion, worsening insulin resistance.
How Puberty Affects Juvenile Diabetes: The Core of Hormonal Challenges
Juvenile Diabetes and Puberty: Hormonal Challenges primarily stem from insulin resistance caused by puberty-related hormones. In normal adolescents, insulin resistance peaks in mid-puberty, reducing sensitivity by up to 30%. In type 1 diabetes, this resistance is more severe, with elevated GH pulses contributing to post-receptor defects in insulin action.
Growth hormone, released in pulses especially at night, counteracts insulin, leading to the “dawn phenomenon”—elevated morning blood sugars. Sex hormones add to this: estrogen and testosterone increase insulin needs, while menstrual cycles in girls cause variable resistance, often peaking mid-cycle or during bleeding.
Glycemic control often worsens, with HbA1c levels rising higher than in other life stages. Adolescents may require 1.5 units of insulin per kg body weight daily compared to 1 unit pre-puberty. Behavioral factors, such as irregular meals, stress, and reduced adherence, compound Juvenile Diabetes and Puberty: Hormonal Challenges.
The Role of Growth Hormone in Juvenile Diabetes and Puberty: Hormonal Challenges
Growth hormone plays a central role in Juvenile Diabetes and Puberty: Hormonal Challenges. During puberty, GH promotes growth but induces insulin resistance in muscle and fat tissue. In type 1 diabetes, portal insulin deficiency reduces hepatic GH sensitivity, lowering IGF-1 production and triggering excessive GH secretion via negative feedback. This cycle exacerbates resistance and promotes ketogenesis, increasing risks of diabetic ketoacidosis.
This diagram shows GH’s multi-organ effects, including increased lipolysis, glucose production, and insulin resistance—effects amplified in type 1 diabetes during puberty.
Symptoms and Signs of Hormonal Challenges in Juvenile Diabetes and Puberty
Teens with Juvenile Diabetes and Puberty: Hormonal Challenges may experience frequent high blood sugars, unexplained lows, increased fatigue, mood swings, irregular periods in girls, delayed growth, or recurrent ketoacidosis. Parents often notice rising HbA1c, more insulin dose adjustments, or emotional distress from fluctuating levels.
Managing Juvenile Diabetes During Puberty: Practical Strategies
Effective management of Juvenile Diabetes and Puberty: Hormonal Challenges requires close collaboration with a diabetes care team, including endocrinologists, educators, and psychologists.
- Frequent Monitoring and Insulin Adjustments — Continuous glucose monitors (CGMs) and insulin pumps help track patterns. Basal rates may need nighttime increases to combat the dawn phenomenon. Bolus doses adjust for meals and hormones.
A young person using a CGM to monitor blood glucose in real time, a key tool for navigating Juvenile Diabetes and Puberty: Hormonal Challenges.
- Diet and Exercise — Consistent carbohydrates, balanced meals, and regular physical activity improve sensitivity. Avoid skipping meals or excessive alcohol, which can cause severe lows.
- Psychosocial Support — Puberty brings independence struggles and peer pressure. Encourage gradual self-management, regular check-ins without nagging, and peer support groups or camps.
- Regular Medical Follow-Up — Schedule frequent appointments to adjust therapy, screen for complications (e.g., thyroid issues), and address mental health.
Optimizing control prevents delays in puberty and reduces long-term risks like retinopathy or nephropathy.
Psychological Aspects of Juvenile Diabetes and Puberty: Hormonal Challenges
Mood swings from brain remodeling and blood sugar fluctuations heighten risks of depression, anxiety, or eating disorders. Girls may face higher risks of disordered eating, such as insulin omission for weight control. Supportive communication and professional counseling are vital.
Success Stories: Overcoming Juvenile Diabetes and Puberty: Hormonal Challenges
Many teens successfully navigate Juvenile Diabetes and Puberty: Hormonal Challenges with resilience and support.
Yesica Mercado Munoz was diagnosed at age 10. During adolescence, she faced severe hypoglycemia incidents and social challenges but learned to advocate for herself. Now in her 20s, she thrives as a university student pursuing a career in pediatric endocrinology, crediting her care team and personal growth for turning challenges into strengths.
Another inspiring example involves teens who, through consistent CGM use and family support, maintain stable HbA1c levels despite hormonal surges. Many participate in diabetes camps, gaining peer connections that normalize their experience and build confidence in managing Juvenile Diabetes and Puberty: Hormonal Challenges.
These stories highlight that with proactive care, teens can achieve normal growth, academic success, and emotional well-being.
Disclaimer
This article on Juvenile Diabetes and Puberty: Hormonal Challenges is for informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized guidance on managing type 1 diabetes, especially during puberty. Individual experiences vary, and self-adjusting insulin or treatment without medical supervision can be dangerous.
Frequently Asked Questions (FAQs)
1. Does puberty always worsen blood sugar control in juvenile diabetes? Yes, Juvenile Diabetes and Puberty: Hormonal Challenges often lead to higher insulin needs and fluctuations due to hormones, but good management minimizes this.
2. Can type 1 diabetes delay puberty? Poorly controlled diabetes may delay puberty onset or progression, but optimal control usually allows normal timing.
3. How much does insulin resistance increase during puberty? Insulin needs can rise by 30–50%, with resistance peaking mid-puberty.
4. What role does growth hormone play in Juvenile Diabetes and Puberty: Hormonal Challenges? GH induces resistance and contributes to the dawn phenomenon; excessive pulses in type 1 diabetes worsen control.
5. Are there tips for parents supporting teens with Juvenile Diabetes and Puberty: Hormonal Challenges? Encourage independence gradually, use CGMs, set non-judgmental check-ins, and connect with support groups.
6. Can exercise help with Juvenile Diabetes and Puberty: Hormonal Challenges? Yes, regular activity improves insulin sensitivity and helps stabilize levels.
7. What about menstrual cycles and diabetes? Cycles cause variable resistance; tracking helps predict adjustments.
8. Is psychological support important during Juvenile Diabetes and Puberty: Hormonal Challenges? Absolutely—depression and eating disorders are more common; early intervention is key.
References
- Puberty and type 1 diabetes. PMC – NIH. https://pmc.ncbi.nlm.nih.gov/articles/PMC4413391
- Type 1 diabetes and puberty. diabinfo.de. https://www.diabinfo.de/en/living-with-diabetes/type-1-diabetes/diabetes-in-everyday-life/adolescents-and-puberty.html
- Supporting a Teenager With Type 1 Diabetes. Breakthrough T1D. https://www.breakthrought1d.org/t1d-resources/relationships/supporting-teenagers-with-t1d
- Thriving with type 1 diabetes — Yesica’s story. Children’s Minnesota. https://www.childrensmn.org/blog/thriving-type-1-diabetes-yesicas-story
- Additional sources from Mayo Clinic, WebMD, and CDC on type 1 diabetes management in children and adolescents.